Medicaid Compliance Plan Template
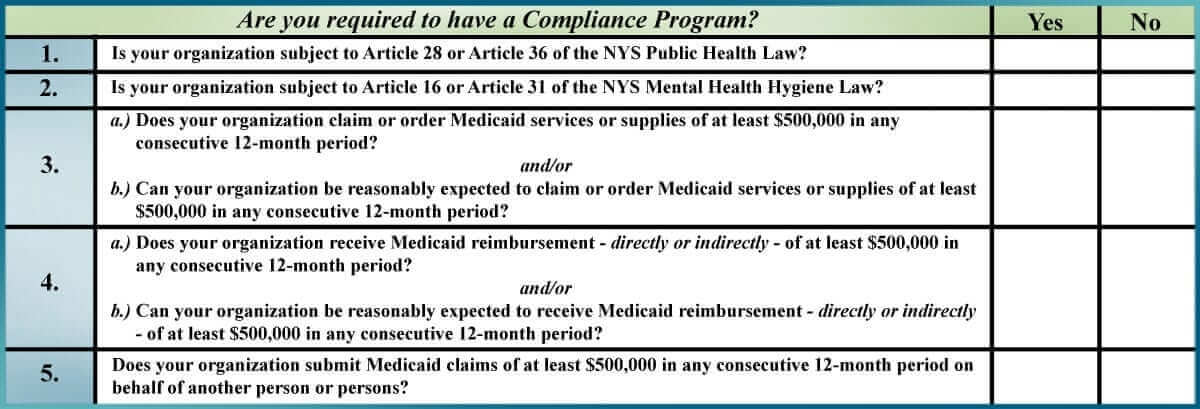
Under that regulation state agencies such as omh are required to implement an effective medicaid compliance program.
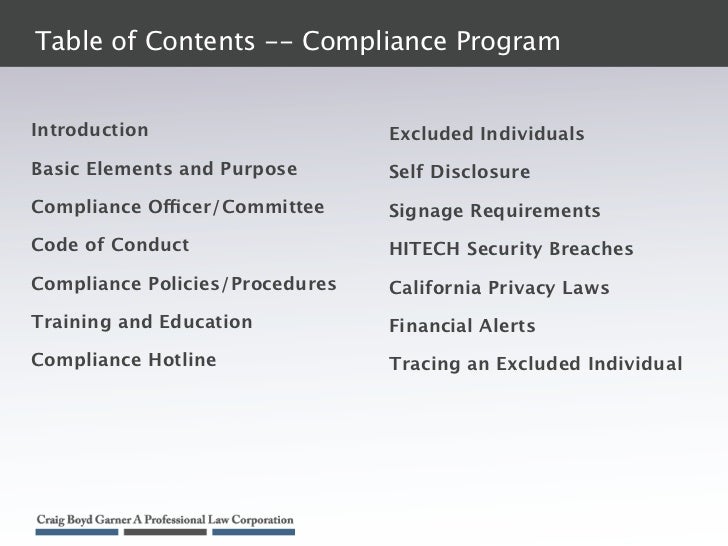
Medicaid compliance plan template. This plan is an integral part of the universitys ongoing efforts to achieve compliance with federal and state laws relating to billing for clinical services. A new part 521 entitled provider compliance programs has been added to title 18 of the codes rules and regulations of new york state. In conjunction with initial and annual training on the compliance plan all immediadent employees will be trained annually on the federal and state false claims act and. The compliance plan and any updates will be on our immediadent website.
Medicaid dollars are used. The medicare compliance plan is a component of care n cares overall compliance program and reinforces the companys commitment to comply with all applicable federal and state regulations as. Medicaid compliance program notice to omh employees. This section contains information related to the cms compliance program policy and guidance and will assist medicare plans and the public in understanding part c and part d compliance program requirements.
Medicaid or other government beneficiaries may violate applicable law. We also consider compliance with regulations to be a subset of our objective of maintaining the highest standards of moral and ethical conduct. Compliance requires a team effort and a mechanism for inquiriesreporting investigating and resolving potential issues. It is the intent of the compliance plan to facilitate that process.
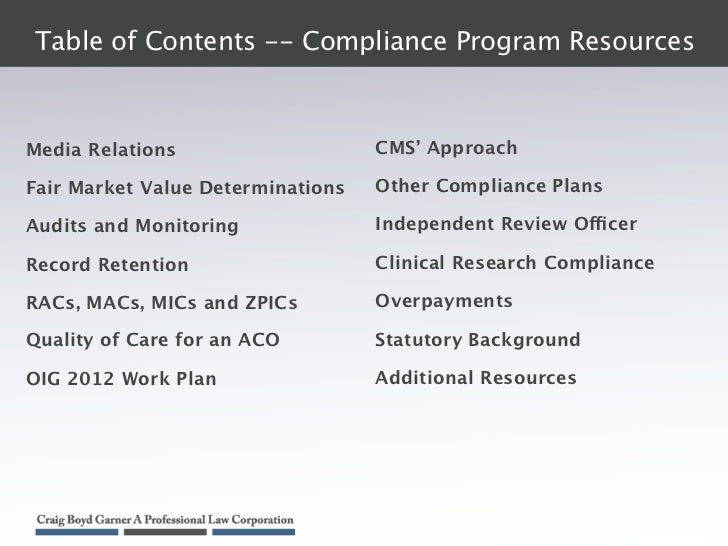
Oig has developed a series of voluntary compliance program guidance documents directed at various segments of the health care industry such as hospitals nursing homes third party billers and durable medical equipment suppliers to encourage the development and use of internal controls to monitor adherence to applicable statutes regulations and program requirements. Omig website the office of medicaid inspector general website contains valuable information on provider compliance programs self disclosure guidance reporting medicaid fraud and other important information such as requirements for verifying new staff members have not been excluded from participating in the medicaid program. Our organization has adopted this corporate compliance plan to comply with the provisions of the deficit reduction act of 2005 nys office of medicaid inspector general work plan social services law 363 d and the office of inspector general of the department of health and human services.